With 1 in 3 patients believing that stents are more painful than stones1, ureteral stents are widely feared and dreaded within the kidney stone patient community. What exactly are stents and how can you minimize stent pain? Here’s your basic guide to all things stent-related.
What are ureteral stents?
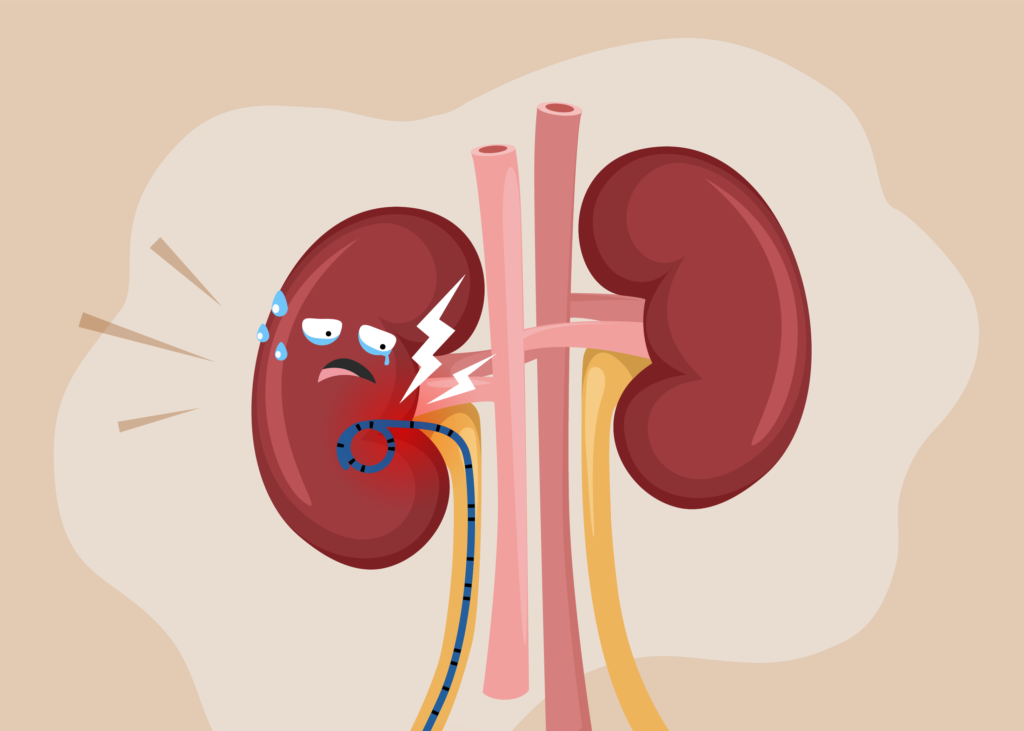
Your ureters play an essential role in draining the urine from your kidneys to your bladder. If you have ureteral obstruction due to a tumor, ureteral stones, or kidney stones, your urine may not be able to drain normally. To hold your ureters open and let urine flow from the kidneys to the bladder, ureteral stents are inserted in your ureters.
Ureteral stents are hollow plastic tubes inserted into the ureter to keep the pathway open and allow passage of urine from the kidney and the bladder. These stents are hollow tubes made with flexible plastic material. For adults, ureteral stents are typically between 10 to 15 inches. Both ends of a ureteral stent are coiled, the top curled end sits in the kidney and the opposite end sits inside the bladder2.
When will a stent be inserted?
Ureteral stents are inserted in the ureter when the normal flow of urine from the kidney to the bladder is blocked. Sometimes, a ureteral stent is also placed to prevent the blockage that stops the urine from flowing. Insertion of a ureteral stent helps to relieve pain associated with the blockage, such as from kidney stones, and makes it easier for urine to pass down the ureter.
You may get a ureteral stent when you have an infection caused by a kidney stone. In this case, a ureteral stent drains the infected urine. A stent may also be placed after you undergo a kidney stone surgery, such as URS. After the procedure, your ureter may swell, and a stent helps to relieve urinary obstruction, ensuring that you have a smoother recovery process3.
What are some symptoms that I can expect after ureteral stent placement?
As your stent sits within your urinary system, urinary symptoms and some changes to your urinary patterns can be expected. Common symptoms include4
- Pain in bladder, abdominal, groin or back area
- Increased frequency of urination
- Feeling of urinary urgency (i.e. having to urinate repeatedly within 15 minutes)
- Urge incontinence (i.e. feeling a sudden need to urinate and being unable to hold it in)
- Burning sensation during urination
- Incomplete emptying of bladder
- Weaker urine stream
These symptoms should subside once the stent is removed.
Why do stents hurt so much?
If you’re experiencing stent pain, you’re definitely not alone. Majority of patients with ureteral stents experience some form of urinary symptoms or pain, with 70% experiencing pain severe enough to affect their daily activities4.
Even though multiple studies have been conducted, the exact causes of stent pain remain largely unknown. Urologists often believe that it is due to the position of the stent within your urinary system.
Since the distal curl of the ureteral stent touches the lining of your bladder, it may irritate the lining of the bladder (bladder mucosa) and cause symptoms like pain and discomfort. Frequency and urgency of urination may also cause a movement in the stent, resulting in further bladder irritation4.
What are some warning signs that I should look out for?
Complications can arise with stent placement. If you’ve had a stent placed recently, keep an eye out for the following symptoms and seek medical attention immediately if any arise:
- Blood clots in urine
- Inability to pass urine
- Severe pain that cannot be relieved with medication
- Persistent fever over 101 °
How can I manage my stent pain?
Over-the-counter NSAIDs are typically effective in relieving stent-related pain symptoms. In the days after a stent placement, try limiting any heavy physical activity to minimize further irritation to your bladder.5
In summary
While stents may cause some discomfort, they are oftentimes a “necessary evil” to keep your ureters and kidneys healthy while recovering from kidney stone surgery. If you’re experiencing stent pain, NSAIDs may be effective in providing some relief.
Sources:
-
2022 Dornier Global Urology Survey (2022). Dornier MedTech. https://www.dornier.com/worldkidneystoneday/
-
Al-Aown, A., Kyriazis, I., Kallidonis, P., Kraniotis, P., Rigopoulos, C., Karnabatidis, D., Petsas, T., & Liatsikos, E. (2010). Ureteral stents: New ideas, new designs. Therapeutic Advances in Urology, 2(2), 85–92. https://doi.org/10.1177/1756287210370699
-
Assimos, D., Krambeck, A., Miller, N. L., Monga, M., Murad, M. H., Nelson, C. P., Pace, K. T., Pais, V. M., Pearle, M. S., Preminger, G. M., Razvi, H., Shah, O., & Matlaga, B. R. (2016). Surgical Management of Stones: American Urological Association/Endourological Society guideline, part II. Journal of Urology, 196(4), 1161–1169. https://pubmed.ncbi.nlm.nih.gov/27238616/
-
Joshi, H. B., A. Stainthorpe, R. P. MacDonagh, F. X. Keeley, and A. G. Timoney. “Indwelling ureteral stents: evaluation of symptoms, quality of life and utility.” The Journal of urology 169, no. 3 (2003): 1065-1069.
-
Turney, B. (2019). Ureteric Stent – Information for Patients. Oxford University Hospitals NHS Foundation Trust.